
Getting the right amount of sleep is important for people with epilepsy. Other epilepsies that occur primarily during sleep include autosomal dominant nocturnal frontal lobe epilepsy, Lennox-Gastaut syndrome, and epilepsy with continuous spike-wave in sleep (CSWS). Fortunately, most children with this syndrome have less than five seizures before going into remission. Approximately 70% of seizures occur during sleep with another 13% occurring as the child wakes up.
Around 20% of people with epilepsy only have seizures during sleep, while 40% only have seizures while awake and 35% have seizures both while awake and asleep. Epileptic Seizures While SleepingĮpileptic seizures can occur during any time of day or night. To increase the likelihood of finding these epileptiform abnormalities during an exam, patients may be asked to sleep during one portion of an EEG. These abnormal brain waves can appear as spikes, sharp waves, or spike-wave patterns.Įpileptiform abnormalities are more likely to occur during certain types of sleep, particularly during sleep stages involving non-rapid eye movement (NREM) sleep. Neurologists also look for specific patterns of brain activity on EEGs, called epileptiform abnormalities.
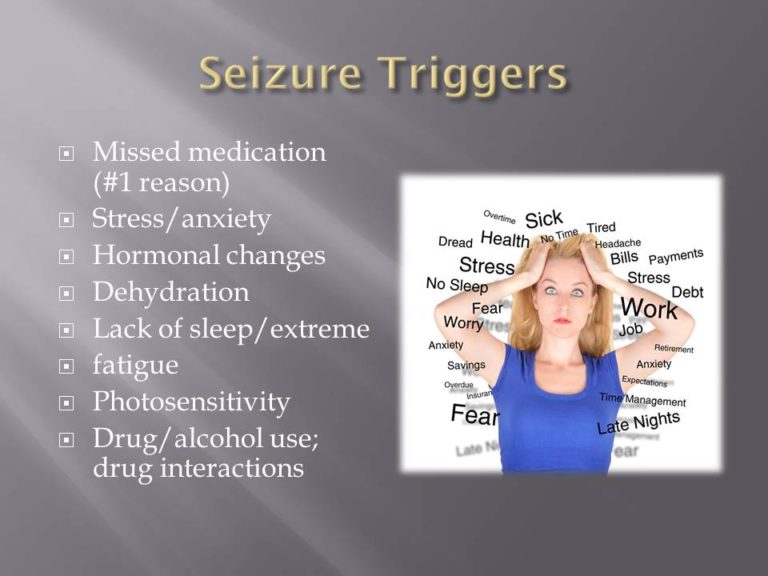
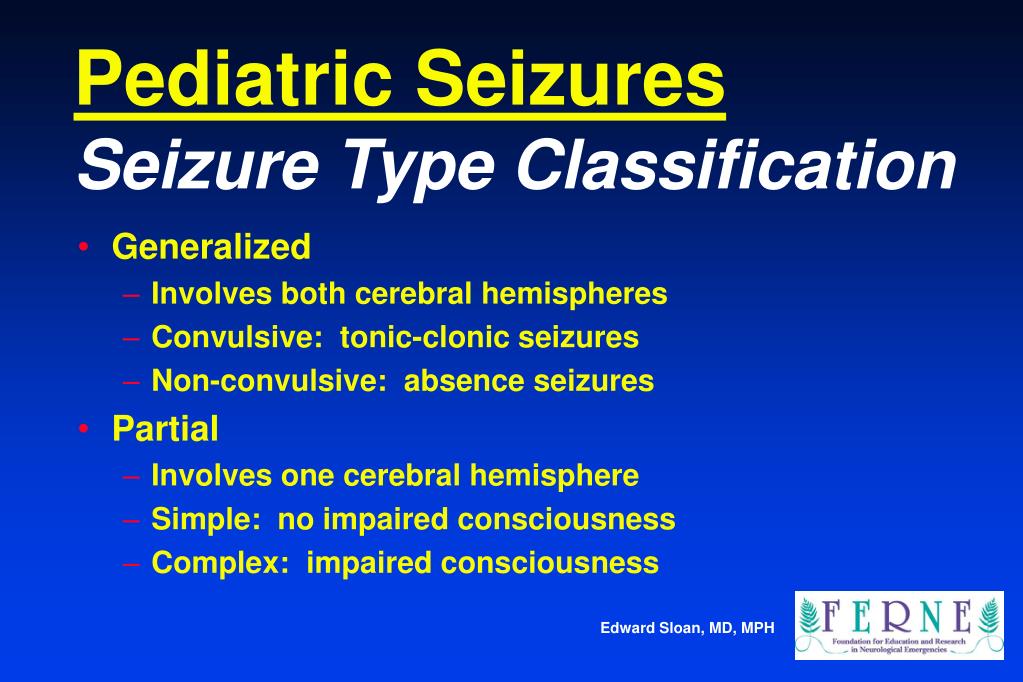
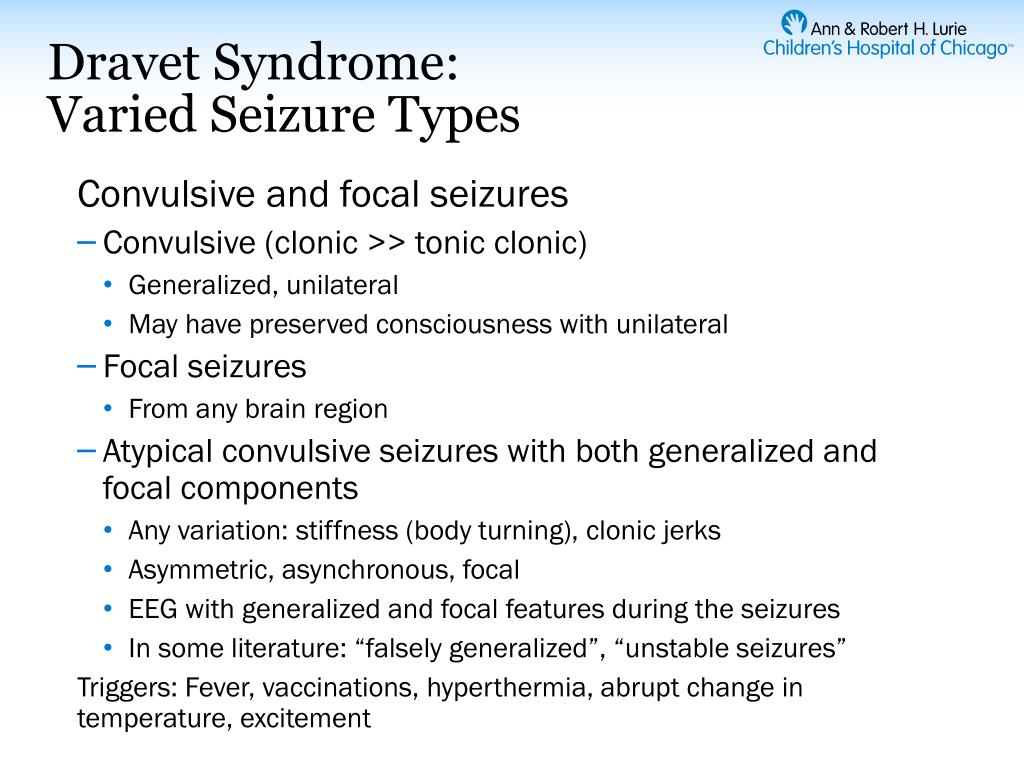
EEGs are used to detect the presence and location of abnormal electrical activity in the brain, which tells doctors if the abnormal activity is coming from all over the brain or from just a small part. When a neurologist evaluates a person having seizures, one tool they use is an electroencephalogram (EEG). While epileptic seizures may be related to medical conditions, brain injuries, abnormal brain development, or an inherited genetic condition, most often the cause is unknown. Diagnosing Epilepsyĭoctors consider a diagnosis of epilepsy when a person has two or more unprovoked seizures at least 24 hours apart. Sleep is a valuable tool in diagnosing epilepsy and research continues to explore the impact that sleep has on the timing and frequency of seizures. Researchers continue to study many important connections between sleep and epilepsy. Aristotle observed this connection in antiquity, and doctors in the late 19th century recognized that most nocturnal seizures occur close to when a person falls asleep and when they are waking up. How Epilepsy Impacts Sleepĭoctors and scientists have long observed a relationship between sleep and epileptic seizures. There are many types of epilepsy and epilepsy syndromes. In people diagnosed with epilepsy, the brain’s electrical activity and connections become abnormal, with sudden bursts of electrical impulses that affect a person’s thoughts, feelings, and actions. Normally, the brain’s electrical activity is relatively orderly. These impulses travel throughout the body using chemical messengers called neurotransmitters. The brain consists of nerve cells that communicate through small electrical impulses. Learning about this complex relationship can help people with epilepsy understand the impact that this condition has on sleep, know the risks of losing sleep, and empower them to take charge of their health. It affects around 1 in 26 Americans and is the 4th most common neurological disorder, after migraines, strokes, and Alzheimer’s disease.Įpilepsy and sleep have a bidirectional relationship, meaning that poor sleep may trigger epileptic seizures and, at the same time, having epilepsy can contribute to sleep issues. Epilepsy is a group of over 30 disorders in which abnormal brain activity causes a predisposition to seizures.


 0 kommentar(er)
0 kommentar(er)
